Gene Therapy to the Rescue
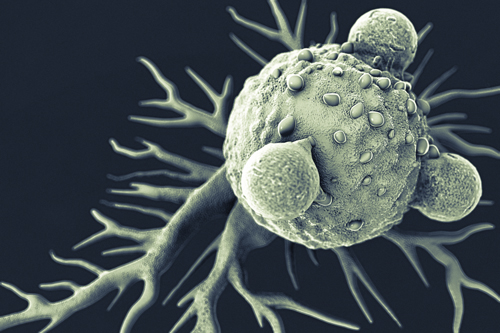
The first investigational oncology gene therapy known as a chimeric antigen receptor (CAR) T-cell therapy is rapidly moving towards FDA approval. These agents — by all means an bioengineering marvel — are constructed from the patient’s own T lymphocytes to escalate their cancer-killing ability, and then re-infused back into the patient. The re-engineered T cells are then directed to kill the cancer cells.
Naturally occurring T cells aren’t always as efficient as they should be in targeting malignancies. Cancers can evade the T-cells, the T-cells become less effective, the T-cells don’t replicate appropriately, and they can miss identifying the tumor target as a foreign body. CAR-T can help to re-invigorate the T cell to do its job.
Learn More: Structure and Mechanism of Action of CAR T-Cell Therapy
The rates of complete response with CAR T in certain leukemias and lymphomas have been impressive, and some patients have been in sustained or partial remissions for years. But it’s important to note studies are still under FDA review, side effects can be serious, and CAR-T is still investigational requiring patient enrollment in a clinical trial.
CAR T-Cell Therapy: Cancer Success
The primary successes seen with CAR T are with refractory hematologic malignancies such as non-Hodgkin lymphomas (NHL) and B-cell leukemias. The C19 tumor target has been the most common tumor target for these cancers. The FDA has already received one CAR T agent biological license application (BLA) for axicabtagene ciloleucel (KTE-C19) from Kite Pharma. It is up for FDA review in 3 subtypes of aggressive B-cell non-Hodgkin lymphoma. A decision is expected in 2017. Promising results have been demonstrated in:
- Aggressive B-cell non-Hodgkin lymphoma (diffuse large b-cell lymphoma, primary mediastinal b-cell lymphoma, and transformed follicular lymphoma)
- Acute Lymphoblastic Leukemia (ALL)
- Mantle Cell Lymphoma
Other cancer types under early phase investigation
Learn More, Including Side Effects of CAR T:
CAR T-Cell Therapy: A Healthcare Professional’s Guide: KTE-C19 Studies