Aggressive B Cell Non-Hodgkin Lymphomas
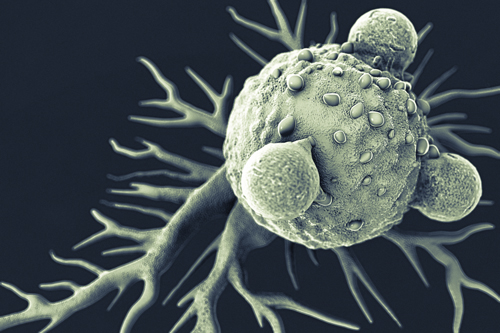
About 90% of lymphoma cases start in the B cells. The C19 tumor target that is sought by the CAR T cell therapy is found on the tumor surface or on B lymphocytes. Other cells are not targeted by the CAR therapy if they do not exhibit the C19 target.
The subtypes of aggressive non-Hodgkin lymphoma submitted in the pivotal trial for axicabtagene ciloleucel (KTE-C19) are:
- Diffuse large B-cell lymphoma (DLBCL) – this is the most common NHL subtype, making up about 30 percent of US cases. DLBCL is aggressive with large masses of B lymphocytes and involves the liver, spleen, bone marrow or other organs. Typically, the treatment for refractory DLBCL is 3rd or 4th line chemotherapy drugs. These patients have a poor prognosis and few treatment options.
- Transformed follicular lymphoma – Follicular lymphoma is the second most common form of lymphoma in the US, and initially may be slow-growing (indolent). However, the risk for transformation to aggressive lymphoma (usually DLBCL) is roughly 30%. A genetic defect, a specific chromosomal abnormality can result in this type of aggressive lymphoma being resistant to standard treatments. Patients with transformed lymphoma who fail standard chemotherapy have a very poor prognosis.
- Mediastinal B-cell lymphoma – This is an aggressive form of DLBCL where a large mass forms in the center of the chest and can compress veins need to carry blood and oxygen to the heart. Roughly 2 to 3% of patients with NHL will have this subtype, usually women in their 30’s or 40’s. Chemotherapy is typically used for treatment; but radiation may also be used.
Pivotal Trial: Aggressive B-Cell Non-Hodgkin Lymphoma
Axicabtagene ciloleucel (KTE-C19) is the first CAR T-cell therapy submitted for FDA approval in the US. The pivotal, multicenter trial submitted by the manufacturer recruited patients with relapsed or refractory aggressive B-cell non-Hodgkin lymphoma (NHL) who were also ineligible for autologous stem cell transplant.
In this pivotal trial known as ZUMA-1, researchers assessed treatment of aggressive refractory B-cell lymphoma with axicabtagene ciloleucel in 101 patients with three subsets of refractory NHL. Here are the major results:
- Objective response rate (ORR) of 82%, the primary endpoint, was met
- ORR at 6 months was 41%, with 36% of patients still in complete response (CR)
- At 8.7 months, the median overall survival was not yet reached, but a meta-analysis of a similar population receiving recommended approved treatments for refractory NHL (SCHOLAR-1 study) had a median OS of 6.6 months.
Relapsed/Refractory Acute Lymphoblastic Leukemia
CAR T-cell therapy is also under research for the treatment of relapsed/refractory acute lymphoblastic leukemia (r/r ALL) in pediatric and adults patients. Axicabtagene ciloleucel (KTE-C19) is in late-stage Phase 1 studies of r/r ALL with Phase 2 studies starting in 2017.
ALL is a cancer of the blood and bone marrow that results in proliferation of immature lymphocytes that are ineffective in fighting infections. In addition, healthy red blood cells from the bone marrow cannot be formed, leading to anemia. There are several approaches to treatment of ALL:
- Blood transfusions
- Chemotherapy, targeted cancer therapy
- Radiation treatment
- Stem cell transplant
Despite these effective treatments, some patients will still relapse over time or be refractory to standard therapy. Investigational CAR T cell therapy has shown impressive results in these difficult-to-treat patients. In the Phase 1 ZUMA-3 and ZUMA-4 trials from Kite Pharma, preliminary analysis found 9 of 11 patients, or 82%, acheived a complete remission or a complete remission with incomplete or partial blood count recovery. In addition, all patients tested negative for minimal residual disease (MRD), which correlates with ALL disease relapse.
Relapsed/Refractory Mantle Cell Lymphoma
Relapsed or refractory mantle cell lymphoma (r/r MCL) is an uncommon, aggressive and often incurable B cell cancer that makes up roughly 6% of non-Hodgkin lymphomas. Treatment initially involves several standard regimens including rituximab (Rituxan). The targeted drug regimen ibrutinib (Imbruvica), a Bruton tyrosine kinase (BTK) inhibitor, was approved in 2013 for patients with relapsed MCL. Autologous stem cell transplantation may also be an option.
CAR T is under research in r/r MCL. Studies at the National Cancer Institute (NCI) have demonstrated durable remissions using CAR T-cell therapy in r/r MCL. In the Phase 2 ongoing single arm, open-label, multicenter ZUMA-2 study from Kite Pharma, investigators will enroll 70 patients with r/r MCL whose disease is refractory to or has relapsed following anthracycline- or bendamustine-containing chemotherapy and anti-CD20 monoclonal antibody therapy and ibrutinib.
The primary objective of this study is to assess safety and efficacy of axicabtagene ciloleucel (KTE-C19) by evaluating overall response rate (ORR) defined as partial remission plus complete remission. Secondary endpoints such as duration of response, progression-free survival, and overall survival are also being evaluated.
Other ZUMA Studies
CAR T-cell therapy has been found to be effective across a wide range of B-cell malignancies. Other ZUMA studiesutilizing the engineered axicabtagene ciloleucel (KTE-C19) regimen include:
- ZUMA-5: Indolent (slow-growing) NHL, with first patient enrollment expected in the first quarter of 2017
- ZUMA-7: 2nd line DLBCL, with first patient enrollment expected in 2017
- ZUMA-8: Chronic lymphocytic leukemia (CLL), with first patient enrollment expected in 2017
Learn more: CAR T-Cell Therapy: A Healthcare Professional’s Guide – Introduction: The Tumor