Hematologic Cancers: On Deck for CAR T
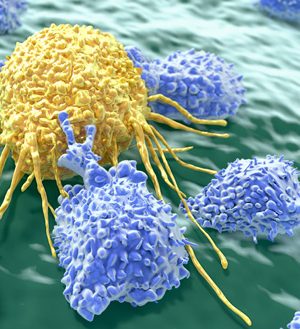
Emerging immunotherapies such as chimeric antigen receptor (CAR) T-cell therapies are some of the most exciting new investigational agents in oncology today. Clinical trial results have been remarkable in refractory leukemias and lymphomas, leading to sustained, high rates of remission in some patients. However, treatments are not without risks.
U.S. Food and Drug Administration (FDA) reviews are moving closer, and decisions are expected in 2017 for hematologic malignancies such as agressive B-cell non-Hodgkin lymphoma (NHL). Other blood cancers under research for CAR T in general include B-cell acute lymphoblastic leukemia (ALL) and chronic lymphocytic leukemia (CLL). Studies are also in process for a wide array of solid tumors such as melanoma or breast cancer, and more follow-up will determine if CAR T-cell therapy is an option for these tumors.
Here, we continue this series to review clinical trials for KTE-C19, a CAR T-cell therapy now up for FDA review.
ZUMA-1: Axicabtagene Ciloleucel (KTE-C19)
Axicabtagene ciloleucel (KTE-C19) from Kite Pharma is an anti-CD19 CAR-T breakthrough therapy currently under FDA review for relapsed or refractory aggressive B-cell non-Hodgkin lymphoma (NHL) in patients who are ineligible for autologous stem cell transplant. This product was initially developed at the National Cancer Institute (NCI). On March 31, 2017, Kite announced they had completed the rolling submission for the Biologics License Application (BLA). If FDA-approved, Kite plans to launch axicabtagene ciloleucel in 2017, and it would be the first commercially available gene therapy.
Kite’s ZUMA-1 pivotal trial assessed treatment of aggressive refractory B-cell lymphoma with axicabtagene ciloleucel in 101 patients (including diffuse large B-cell lymphoma [cohort 1, n=77], and mediastinal B-cell lymphoma and transformed follicular lymphoma [cohort 2, n=24).
After one infusion of axicabtagene ciloleucel, the primary endpoint for the combined groups was met with a statistically significant 82% objective response rate (ORR). At 6 months, the ORR was 41%, with 36% of patients still in complete response (CR). Five of the 101 patients continued to exhibit durable partial responses (PR) with minimal abnormalities in PET scans. One of these PRs converted to a CR at month nine. At 8.7 months, the median overall survival (OS) had not yet been reached, although a similar patient population from the SCHOLAR-1 study had a median OS of 6.6 months.
ZUMA-1 Adverse Events
Axicabtagene ciloleucel (KTE-C19) was granted breakthrough therapy designation for all 3 lymphoma subsets by the FDA in 2015 as it tackles a significant unmet need – patients with aggressive B-cell lymphoma who have run out of treatment options. However, some side effects can be serious. In ZUMA-1, the most common grade 3 or higher adverse events included:
Anemia (43%), thrombocytopenia (24%)
Neutropenia (39%), febrile neutropenia (31%), decreased neutrophil count (32%)
Decreased WBC count (29%), decreased lymphocyte count (20%)
Neurologic events (28%)
Encephalopathy (21%)
Cytokine release syndrome, CRS (13%)
CRS is a serious, potentially fatal, side effect of any CAR-T cell therapy that results in cytokine release causing high fevers, low blood pressure, and neurologic side effects like delirium and confusion. Side effects like CRS and neurotoxicity have been managed with the interleukin (IL-6) inhibitor tocilizumab (Actemra), corticosteroids, and/or supportive care.
Three deaths were reported; 2 deemed related to therapy. One case was reported as hemophagocytic lymphohistiocytosis, where the immune system damages the patient’s own tissues and organs, and one cardiac arrest in the setting of CRS.